The Delta variant initiated a new dawn of the COVID-19 pandemic.
......goin' to take you to His mansion in the sky......
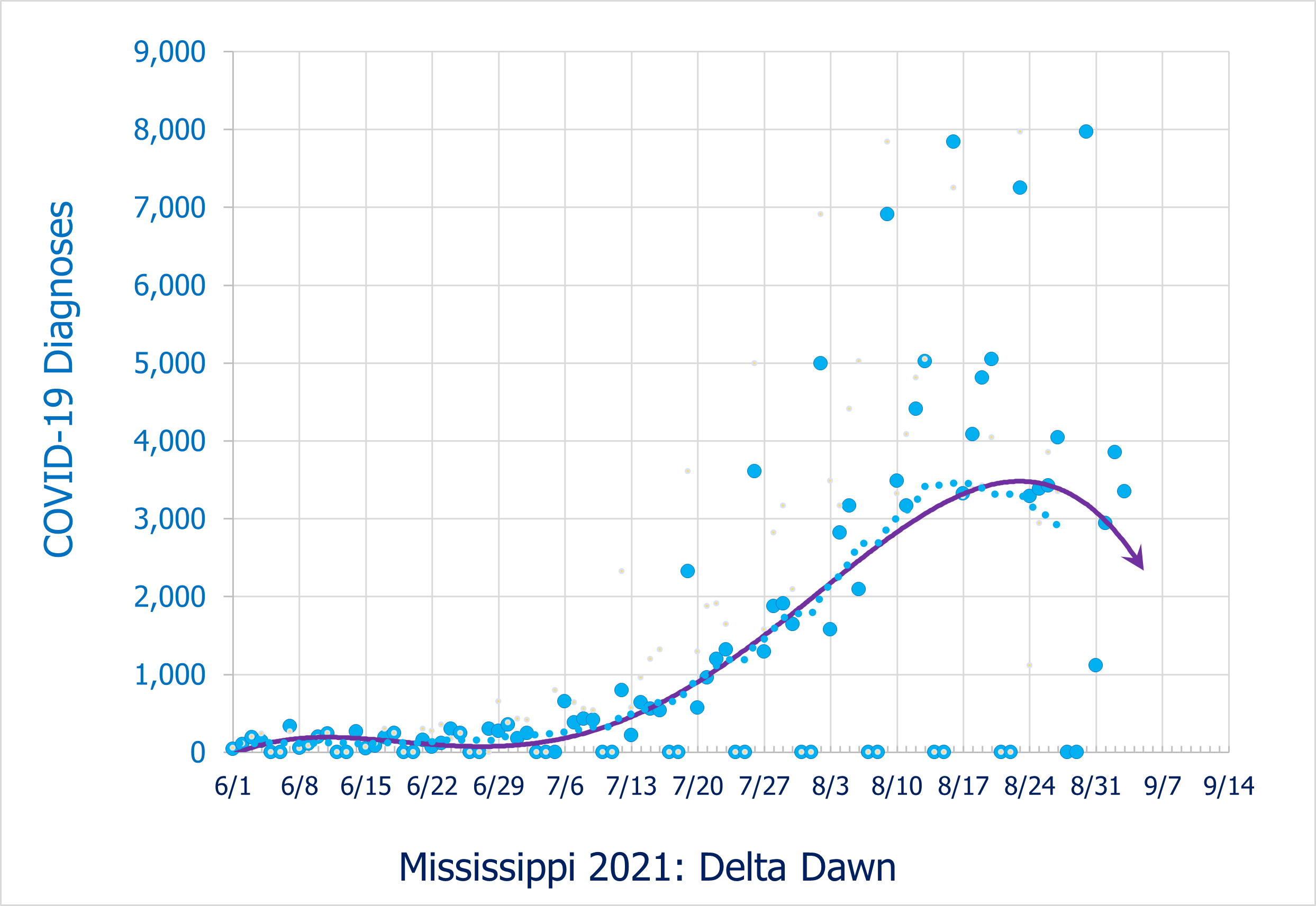
The first 26 cases of the Delta Variant were detected in Mississippi during May, 2021.
To the unwary, this small incursion was of little or no concern.
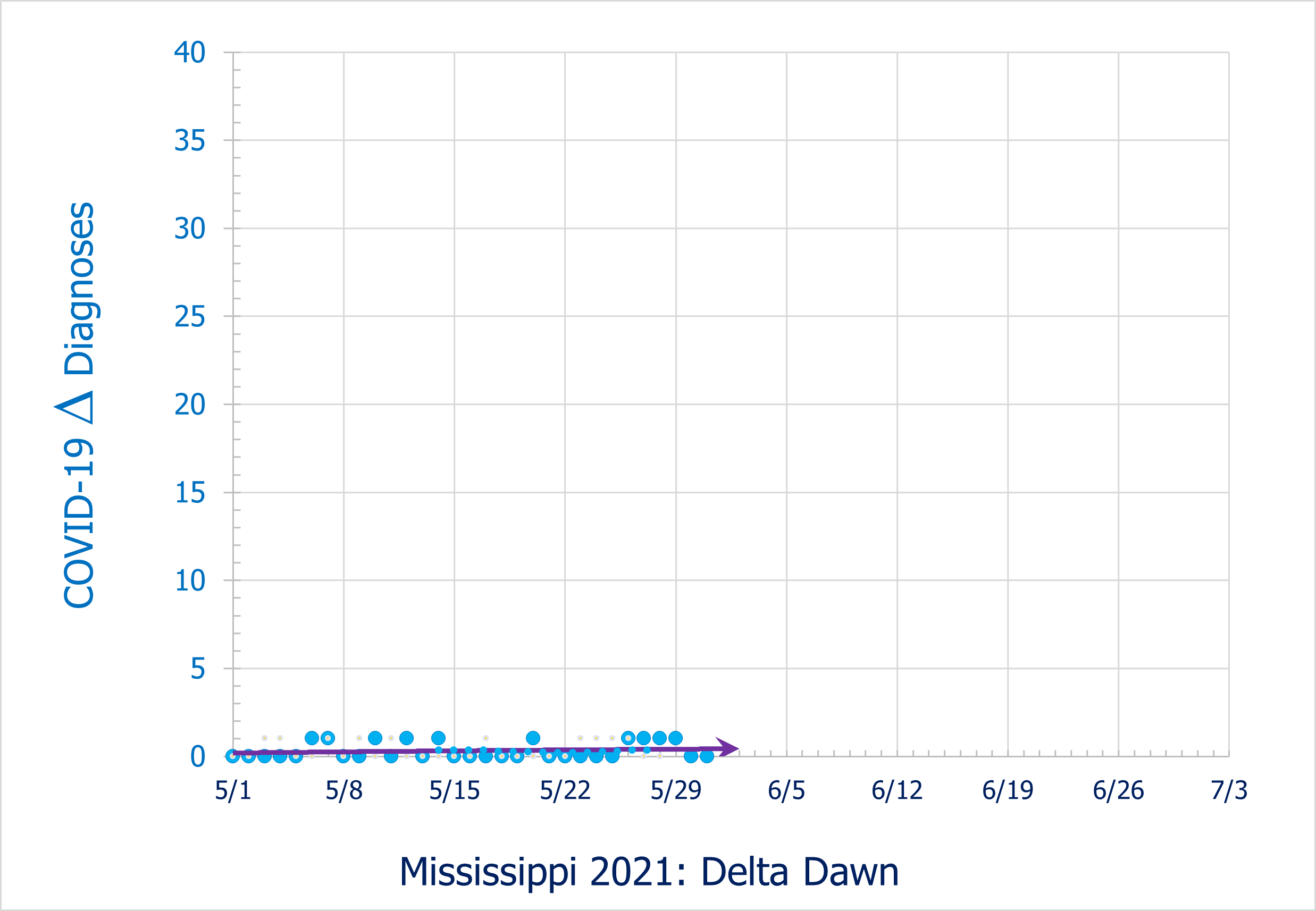
Under the placid surface of a seemingly calm Spring Break from the Covid-19 pandemic, the Delta variant was growing exponentially.
(The solid line is a polynomial fit. The dotted line is the 14 day moving average, retarded by 7 days to align the average with the underlying data)
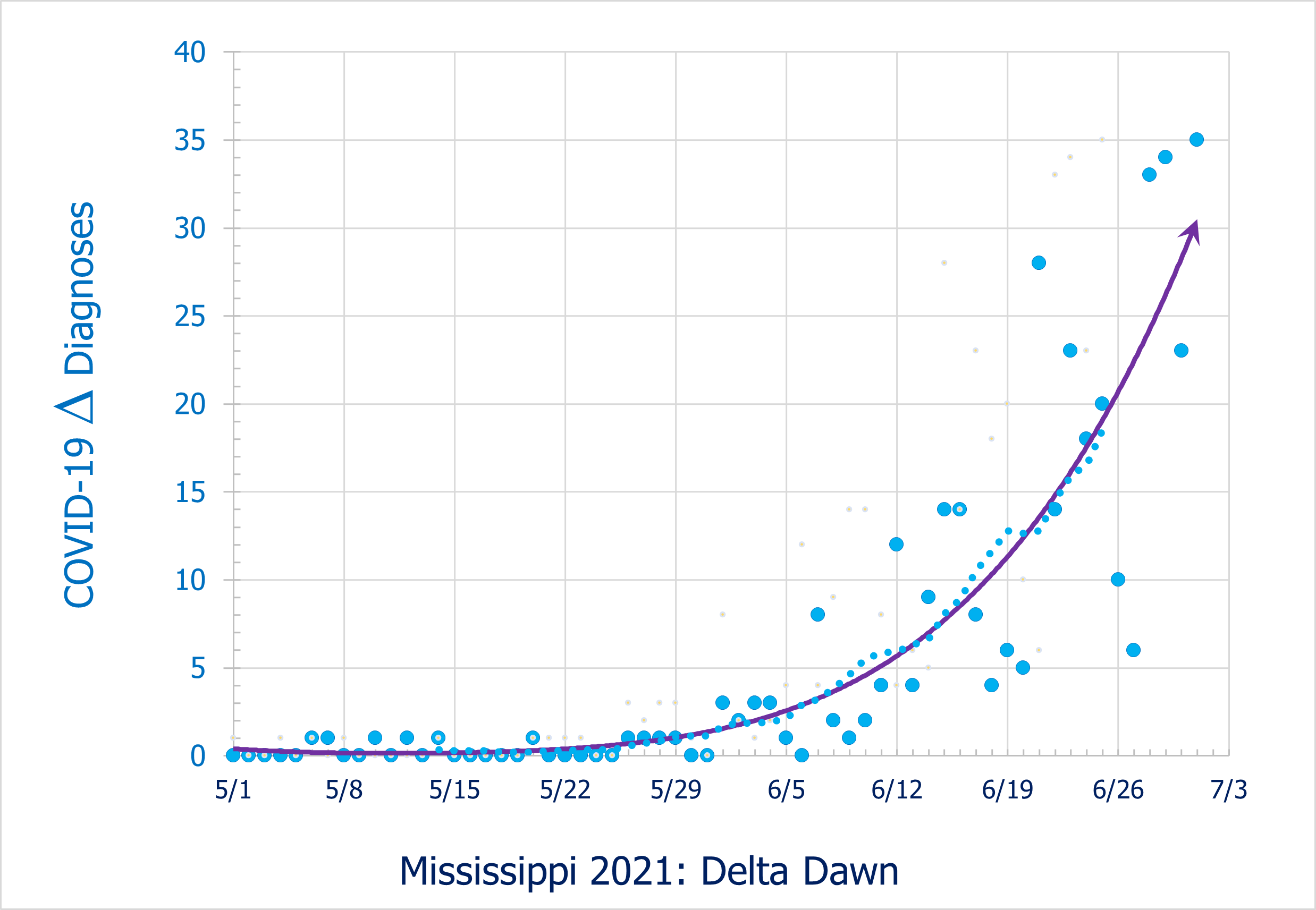
July saw the slow, almost imperceptible growth of the new surge.

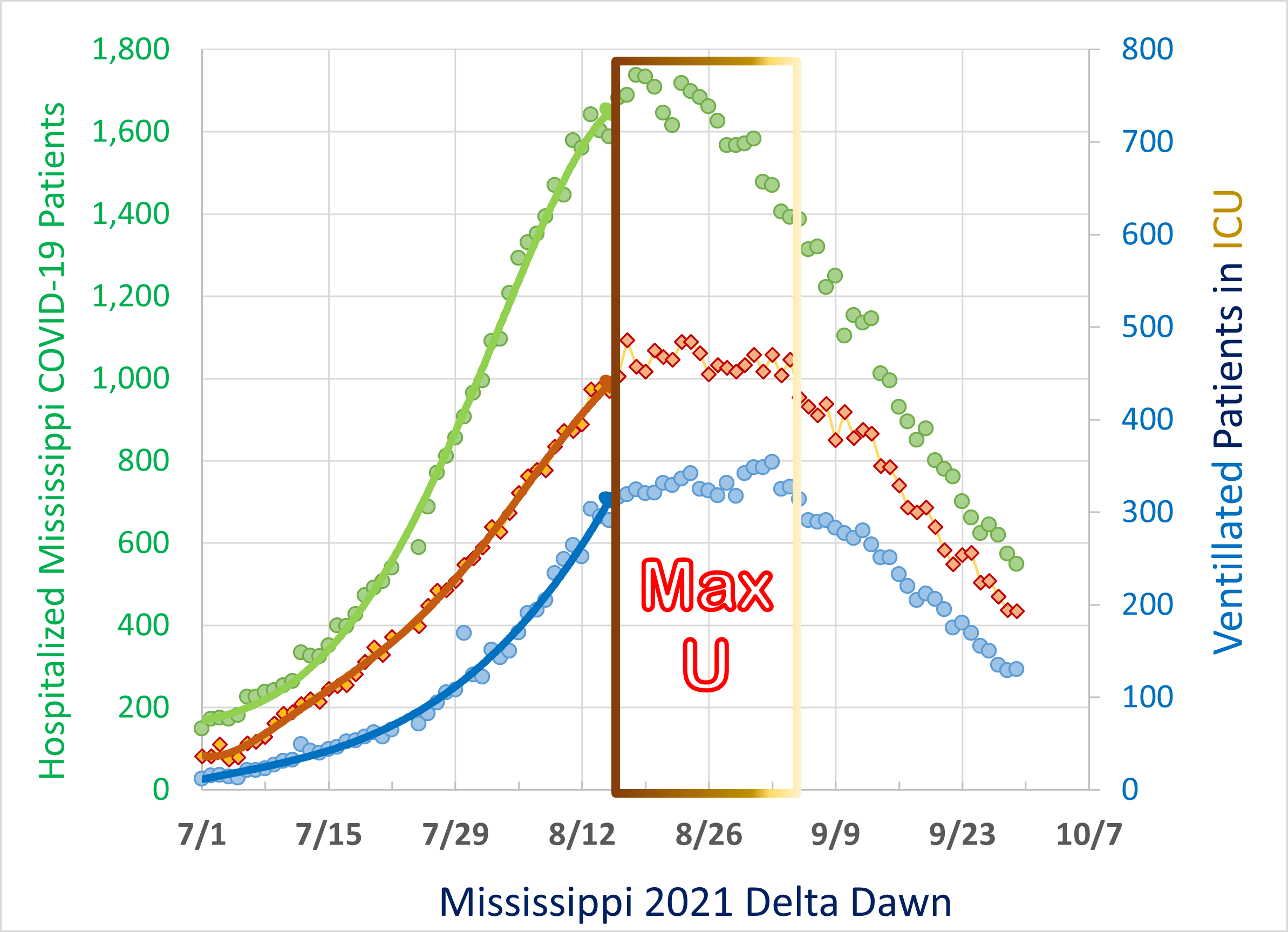
The number of hospitalized COVID-19 patients accelerated through the month of July (green), doubling in the first half of the month and growing to 907 at the month's end.
ICU's filled with COVID-19 patients at a steady pace (orange), and the number requiring ventilation accelerated rapidly in the second half of the month (blue).

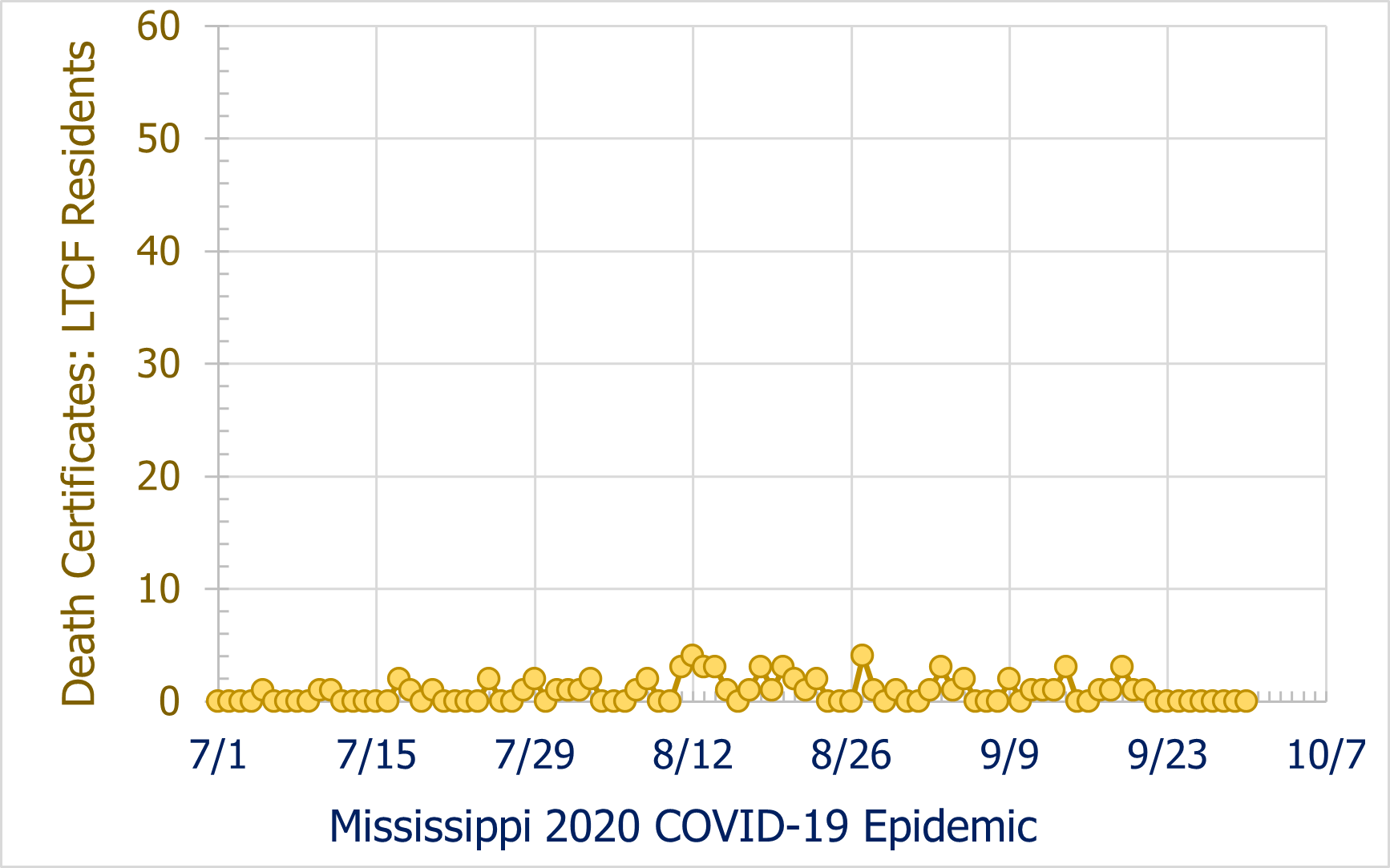
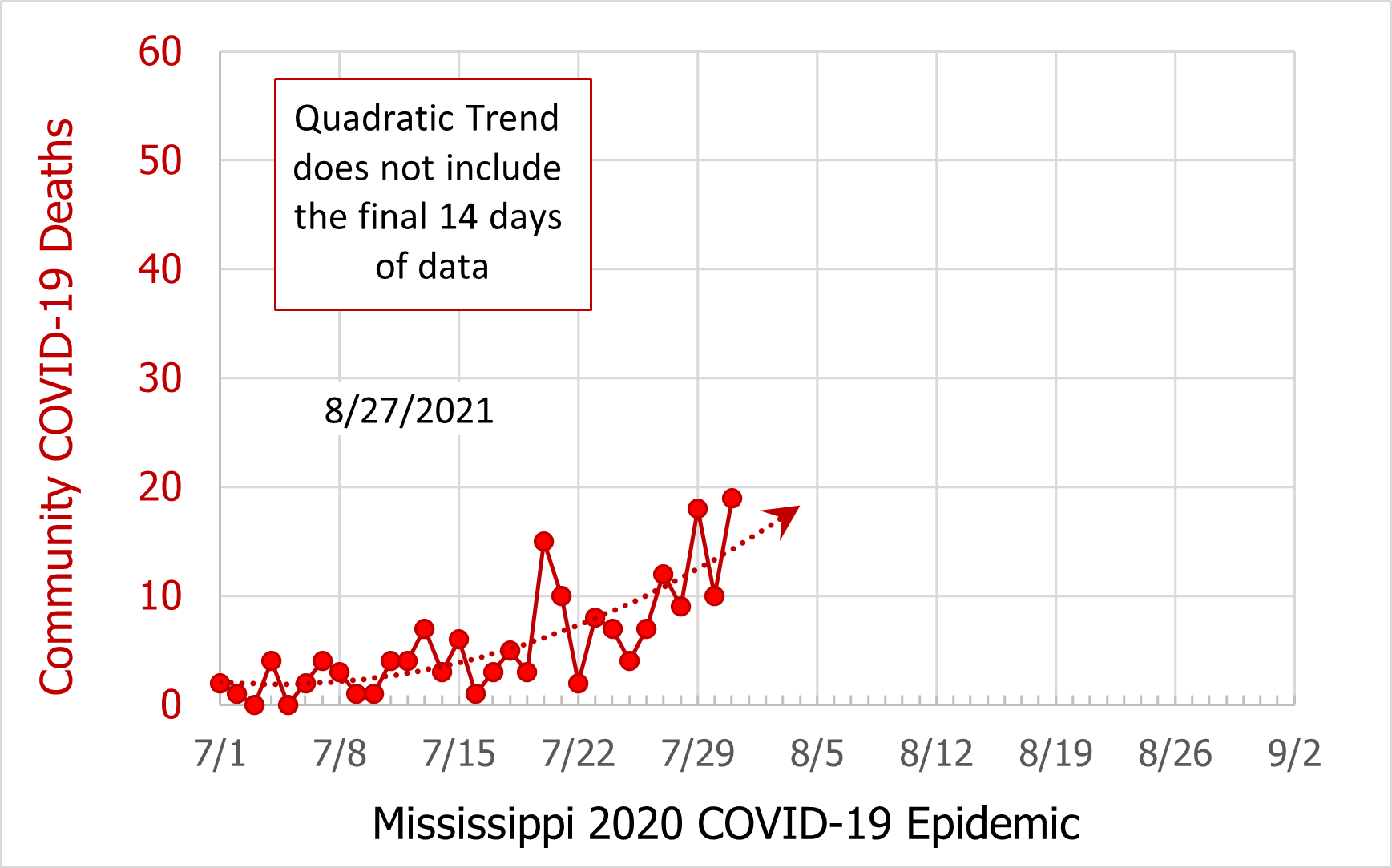
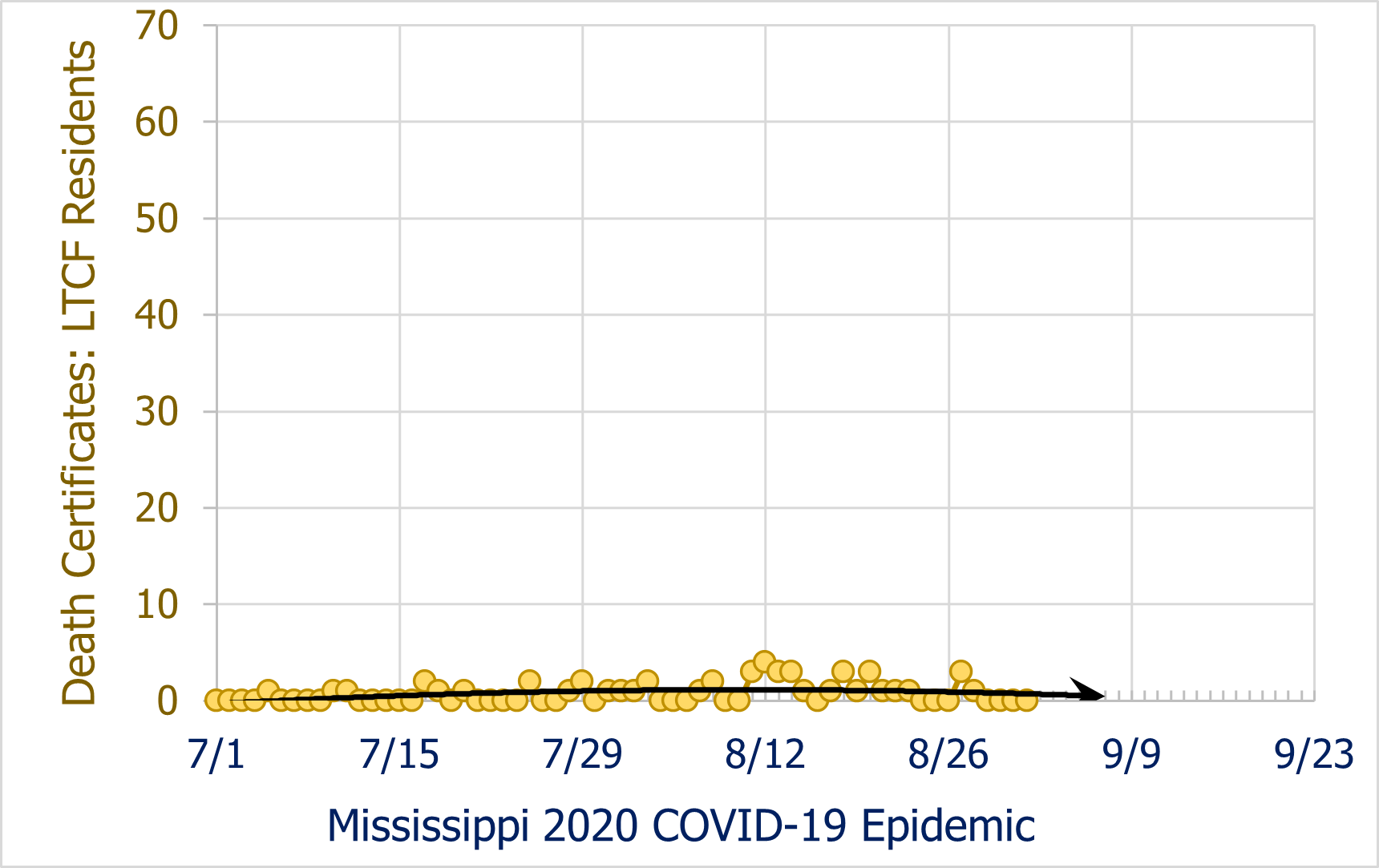
Death certificates hinted at an incipient surge in the community, while individuals in long term facilities were almost entirely protected from COVID-19 related fatalities.

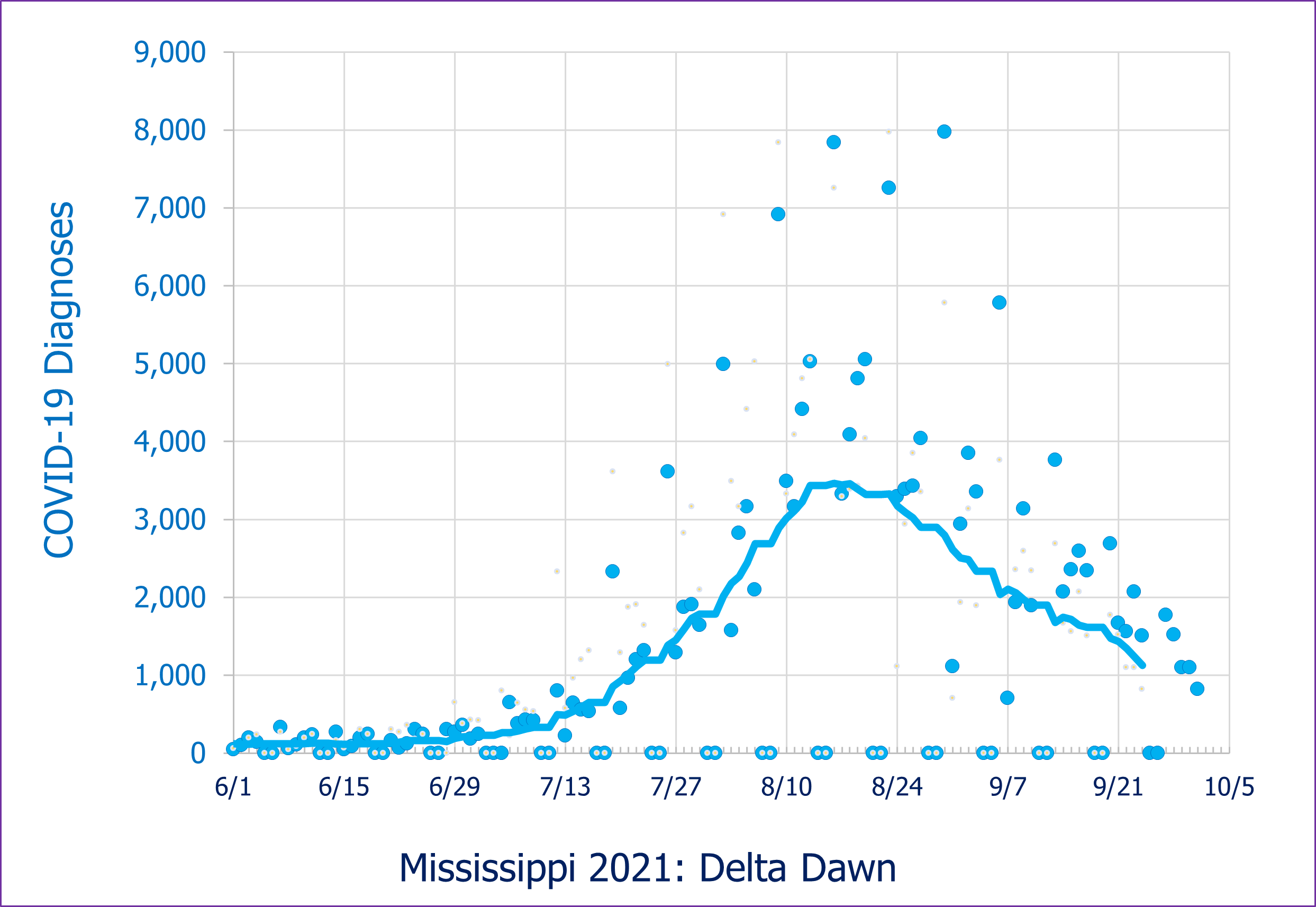
August was bad and confusing day by day.
Diagnostic tests were not reported on the weekends, but instead were summed up and reported on Mondays, so days with outlier high counts followed days with zero counts.
Moreover, Hurricaine Ida prevented adequate testing at the end of the month.
Maximum Utilization of all hospital resources was reached half way through August.
During this pandemic, individual ICU's have been at Max U for extended periods of time. The 4 most extreme cases - as of 9/29/2021 - were the Mississippi hospitals of Meridian (56 weeks), Vicksburg (48 weeks), Oxford (33 weeks) and Greenville (25 weeks). But it was only with the Delta variant that the entire states hospitals were filled to overflowing.

Death certificates documented the COVID-19 mortalities in the community. Data are slow to arrive, even weeks after the month is over, causing an underestimate in the record for the ultimate two or more weeks of the data set. So these incomplete data are plotted separately (dark yellow). The predicted number of deaths not yet reported for this two week period are plotted in grey.
Individuals in long term facilities continued to be almost entirely protected from COVID-19 related fatalities. The protection is not complete, as individual deaths have increased as overall infections rose.

A September to remember.
Diagnosed COVID-19 trended downward through a set of data that were highly scattered due to the manner that they were determined and were reported.
Maximum Utilization eased dramatically for hospitals, with the census falling by half. ICU's census (as well as the number of their ventilted patients) also abated.
Two factors contributed to this pattern.
1. Fewer people with Covid-19 are sick enough to require hospitalization.
2. The less ill recovered and were discharged.
3. Mississippi's ICU's were inadequate to care for all the seriously ill COVID-19 patients - the ICU's took who they could, but others had to wait. Deaths of patients in this waiting list also reduced the hospital census.
Deaths - the most objective measure of the pandemic - plateaued and showed signs of decline.
(Death certificates documented the COVID-19 mortalities in the community. Data are slow to arrive, even weeks after the month is over, causing an underestimate in the record for the ultimate two or more weeks of the data set. So these incomplete data are plotted separately (dark yellow). The predicted number of deaths not yet reported for this two week period are plotted in grey.)
(Individuals in long term facilities continued to be almost entirely protected from COVID-19 related fatalities. The protection is not complete, as individual deaths increased in mid August, then fell back.)